#RightInhalerImage campaign
Inhalers are frequently portrayed in the media incorrectly leading to misconceptions about their use. We know lung diseases are responsible for more than 700,000 hospital admissions in the UK each year. One in five people have a respiratory disease and half of these people manage their condition with inhalers.
We have convened a large group of expert respiratory heath care professionals from across the UK who have united to address their concerns about the way asthma inhalers are portrayed in the media. We have observed that most images used by the media depict incorrect use of inhalers, therefore continually re-enforcing the wrong messages to people with asthma who rely on these vital treatments.
The #RightInhalerImage Campaign aims to improve the quality of media portrayal of inhalers which we believe would improve information for patients, health care professionals and the public about the use of inhalers. To achieve this, we are campaigning to ensure images represent inhalers being used correctly and would love you to join us.
We invite you to work with us on this campaign. What action can you take?
- Join our social movement for change #RightInhalerImage which commences on World Asthma Day May 5th 2021.
- Pledge to use appropriate images.
- Support us in asking the media to remove inappropriate images from publications when asked.
- Use resources from the communication toolkit below to raise awareness of this campaign amongst your networks
Please find resources to support your local campaign in our #rightinhalercampaign communications toolkit.
The right image matters
Positive images of children, young people and adults using inhalers correctly will go a long way to help improve the care and outcomes for our population.
People with asthma usually need two different inhalers: a preventer (brown, pink, red, orange etc.) and a reliever (generally blue). The preventer inhaler is often forgotten about but is one of the most important parts of asthma treatment. A pMDI also known as a “puffer”, is the most common inhaler device used in the UK. There are lots of different coloured devices, and the colour indicates the type of medicine inside the inhaler. If images depicting preventer inhalers are used rather than blue inhalers this demonstrates good asthma management and might help contribute to a reduction in global warming.
Over promotion of reliever (blue) inhalers reinforces a perception that this is the most important inhaler. However, from the National Review of Asthma Deaths in 2014 we have evidence that overuse and reliance on blue inhalers was frequently a causal factor in mortality.
Images portraying incorrect inhaler use may contribute to the adoption of poor inhaler technique and counteract medical advice. We want media images to portray the best guidance for people with asthma and you can help us.
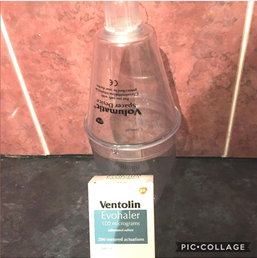
Right images with spacers
Child with a spacer
Child with a facemask
Adults
You can also find additional images on the IPCRG gallery of approved images: https://www.ipcrg.org/gallery
Spacers
Inhalers are not always easy to use, and correct technique is important to ensure the medicine is deposited in the lungs where it is needed. Spacer devices make pressurised Metered Dose Inhalers (pMDI) much easier to use and help the medicine deposition. Images in the media need to reflect this for both children and adults. Incorrect images are contributing to the adoption of poor inhaler technique and counteract medical advice, something that has been seen clinics.
Find more information on spacers from Asthma + Lung UK.
Other resources
Inhaler Images taking Clinical tips
Asthma UK: Asthma inhalers, medicines and treatments
UK Inhaler Group: Inhaler Standards and Competency Document
Important to use the right spacer poster
Videos
Campaign teaching slides PowerPoint
Asthma UK – How to use your inhaler videos
UK Inhaler Group: Inhaler Standards and Competency Document
#RightInhalerImage Communication Toolkit
References:
https://statistics.blf.org.uk/asthma
National Review of Asthma Deaths (2014) https://www.rcplondon.ac.uk/projects/national-review-asthma-deaths
Nelson S, (2021) Let’s improve media portrayal of inhalers – Journal of Community Nursing, June p12-13
Guilmant-Farry, Nelson S (2021) Asthma’s image problem. Community Practitioner Vol 94 | No 03 May/June 26-2
Nelson, S, Marsh, V (May 2022) From kick-start to full steam ahead for the #RightInhalerImage Campaign
Blogs
My son’s first asthma attack almost killed him; it came out of the blue, it was terrifying; he was 18 months old.
He was “too young” to be diagnosed with asthma despite plenty of supporting evidence such as having eczema and relevant family history. We left hospital with an inhaler we were told to give him if he were to get wheezy. And that was it! Confused, concerned and anxious but delighted that he had bounced back to his old self, off we went – clueless in hindsight.
My son’s second asthma attack occurred 4 months later; thankfully, we got to hospital quickly and it turned out not to be as bad as the first. 2 days later we went home with a diagnosis of asthma, an orange (preventer) inhaler and new spacer device, and an appointment to see an asthma specialist.
That orange inhaler was magic; what a difference it made. No more cough keeping him awake at night, no more bouts of breathlessness or coughing when he was playing or getting excited. And no more asthma attacks …. actually, there was one more. It happened 6 months later; thanks to all the advice we had been given we recognised it straight away and got him to the GP immediately. This time he did not need to go to hospital, the GP gave him steroids and we looked after him at home. I have no doubt that it was that orange inhaler that made the difference and had he not been on it he would have been really poorly again.
My son is now a young man, he still has asthma, but he is fit, strong and healthy. Through his teenage years he rebelled, he did not want to have asthma and he certainly did not want to take inhalers. There were arguments in our house and plenty of nagging, but we found our way. Over the years the practice nurses were brilliant; they understood he did not want to use a spacer anymore and suggested other inhalers for him to try, and they understood he did not see the need to take his steroid inhaler every day, so they spent time explaining to him how important that was.
Now my son has a dry powder inhaler so no need for a spacer. He still forgets to take it sometimes but if he gets a tight chest and needs to use his rescue (blue) inhaler it reminds him that he needs to take his preventer inhaler every day to stop that from happening. My son was lucky, we were lucky, asthma kills.
#RightInhalerImage campaign – what do I think as a clinical nurse specialist for asthma and allergy – I think so exciting! So needed! So crucial!
Considering asthma is the most common chronic disease in childhood, affecting 1 in 10 children in the UK (NICE, 2017) – how can it be that media images are often completely inaccurate and just wrong! This seriously fuels the battle we have as health professionals to improve asthma standards and care in the UK, for which we are failing. The Global Asthma Report (Global Asthma Network, 2018) listed the UK among the worst asthma death rates in Europe. This is shocking!
The use of images promoting incorrect inhaler use gives out the wrong messages to and could negatively impact asthma control, leading to potential asthma attacks and chronic ill health. A typical example is using images of children using metered dose inhalers (press and go/puffer inhalers) without a spacer device. Without a spacer device, at best only 20% of the medication actually reaches the airways – the rest remains in the mouth where it is not clinically effective (Vincken et al. 2018). Not showing spacers with this particular type of inhaler when depicting asthma care, whether in print or within TV shows, has led to ‘spacer ignorance’; people/society are often unaware that spacers are an integral part of inhaler use. This leads to poor compliance with spacer use, as children and young people do not want to stand out, or be perceived as different when using their inhalers. If we can normalise spacer use in the media, this may tackle some of the embarrassment and stigma issues. The #rightinhalerimage campaign will begin to address this, raising awareness and tackling inhaler stigma. However, not including spacers with inhaler images is only one part of the issue.
Frequently inhaler images depict the use of a reliever (rescue) medication; salbutamol which is in a blue inhaler. This image is so commonplace; no one takes any notice if a ‘blue inhaler’ is used. This can be deadly! Overreliance on salbutamol inhalers was identified as one of the key themes associated with avoidable asthma deaths in the National Review of Asthma Deaths (2014). The repeated use of salbutamol inhalers needs to be seen as an alarm that asthma control is lost and medical review is needed. Of course, it’s ok to use the blue inhaler when it is needed (it is rescue medicine), but more than 2-3 times a week should be be regarded as a loss of asthma control and not ignored. #RightInhalerImage can start to address these issues, we can start to put right the asthma messages, building a foundation of awareness and information to pave the way for improved asthma care in the UK. Will you join us?
References
Nice 2017 ………..
Global Asthma Network, 2018…….
Vincken et al. 2018
National Review of Asthma Deaths (2015). https://www.rcplondon.ac.uk/projects/national-review-asthma-deaths
The #RightInhalerImage campaign and its importance to me
I started to develop allergies to our dog, my best friends cat and dust as a child and during my late teenage years it was obvious I had hay fever. I manged this mainly by avoiding the triggers particularly the housework wherever possible! I had my first nasal polypectomy at 16, but no one linked this to the fact I could have asthma!
I was provided with a blue reliever inhaler to help the occasional wheeze. Some years later whilst working at a world-renowned London hospital it was rightly suggested I had mild asthma and should add in a brown ‘preventer’ inhaler to my repertoire, but just in the winter months or during the pollen season, whenever I felt the need. At some point I saw the light and realised that perhaps the brown inhaler should be taken a little more regularly and despite years of denying it I had to accept I did in fact have asthma. Looking back there were a few scary moments in the nurse’s home when I perhaps should have gone to the emergency department and I thank my lucky stars that nothing untoward happened. No one told me that asthma could kill, in fact no one really told me much as it was assumed I was a healthcare professional so should know.
It was not until many years later when my then, new GP husband questioned why I did not use a spacer when taking my medication, as this was best practice. I initially pushed back stating my asthma was not bad enough, so I didn’t need to, and after all it hadn’t been recommended by my own GP! We have been married 20 years and I now know he was quite a forward-thinking GP and for once might actually have been right!
This was reinforced when I was asked to lead the London asthma programme for children and young people and heard Dr Mark Levy present the outcomes of the National Review of Asthma Deaths at our first meeting. For once, I was pleased I had actually listened to my husband’s advice! I soon learnt and became almost evangelical about the fact that a spacer helps improve the medicine deposition (Vincken et al, 2018) and whilst not essential for all adults, is key in the management of children and young people.
In recent years, whilst leading this programme, it has become increasingly frustrating to see the use of images promoting incorrect inhaler technique and over promoting the use of the blue reliever inhaler, rather than pictures of preventer inhalers in the media. These give the wrong message and may negatively impact a patients asthma control, leading to potential asthma attacks and worsening quality of life. It is for this reason why we have gathered together a group of leading respiratory health care professionals to launch the #RightInhalerImage campaign to improve the quality of media portrayal of inhalers which we believe would improve information for patients, health care professionals and the public about the use of inhalers. I hope you will join me in being evangelical too and help spread the word!
References
Royal College of Physicians (RCP) (2014) Why asthma still kills: report from the National Review of Asthma Deaths (NRAD) [online]. Available from: https://www.rcplondon.ac.uk/projects/national-review-asthma-deaths [Accessed 13 April 2021].
Healthy London Partnership Asthma programme for children and young people https://www.transformationpartners.nhs.uk/our-work/children-young-people/asthma/
Vincken, W., Levy, M.L., Scullion, J., Usmani, O.S., Dekhuijzen, P.R. and Corrigan, C.J. (2018) Spacer devices for inhaled therapy: why use them, and how? ERJ open research, 4 (2).
The importance of using a spacer – a Parent’s Perspective
As a parent of a child with severe asthma, you’re on a really steep learning curve from day one. This never really ends, because we are both always learning something new. People always assume because of my job that I know it all, but actually it makes it even harder. It’s really hard to be objective when it’s your own child and there are emotions involved!
Both of my girls have asthma, but my eldest daughter (who is now 19) has severe difficult asthma, which lead to an intensive care admission in 2017, and one of the worst times of my life. It’s been quite a journey since then, and now we are at the stage where she has found the right treatment for her, and is beginning to take responsibility for managing her asthma. It is really hard let go though.
My daughters, aged 13 and 19
When I look back to when she was first diagnosed with asthma, at the tender age of 2 years, I vividly remember being given a Salbutamol inhaler by her GP and being told “just give it to her when she needs it”. My husband and I were pretty clueless and inexperienced, so we took the inhaler home, and ended up trying to push it into her mouth when she became unwell. Understandably, she hated it, and so did we.
A spacer device was never mentioned to us, and we didn’t know such a thing existed. If we had, I really believe this experience would’ve been much less stressful for all of us, and of course she would have got better much sooner.
We learned about spacers as she got older, thanks to the amazing Practice Nurse at our GP surgery. By then, I had qualified as a paediatric nurse and was working in a busy emergency department, so I became more familiar with the different types of spacers. The more I learned about asthma in my job, the more I realized how little I had known as a parent. Taking the time to give that little bit of education, can make a HUGE difference.
Since then, spacers have become an essential in our house. We have a variety of spacer devices that live at home, in my car, my daughter’s car, as well as at the school, university and grandparents’ house.
Both of my girls know NEVER to use their inhalers without their spacer, and the reasons why. With two teenagers, there is often a lot of eye-rolling when I say “where’s your spacer??”, but they know!
Spacers are part of the furniture in the Massey house!
The most important thing I would share with other parents is this: using a spacer is ESSENTIAL for taking asthma medication properly. If you don’t use one, you might as well be spraying that asthma medication into thin air, because it certainly won’t be inhaled without one! Looking after your spacer is also very important. I tend to replace ours when they become damaged, and I aim to wash them out once a month in warm, soapy water. Another tip? DON’T be tempted to put them into a dishwasher, it may seem like a good idea, but it WILL damage the spacer, and always let it air dry after cleaning. Face masks have a habit of catching water in their rim, so always give them a little shake to make sure they are fully dry before use. Follow the manufacturer’s instructions and you should be good to go!
If I had to name the top three most important bits of advice for keeping your child’s asthma well controlled, using a spacer would definitely be up there. You can have the best, most effective asthma treatment out there (and be taking it 100% of the time), but if you’re not using your spacer, it’s unlikely to work. Starting these good habits when children are young means they are more likely to keep them as they grow older, and start to take responsibility for self-managing their condition.
Jo Massey, parent
Community pharmacy teams (also known as healthy living pharmacies) can help empower people with asthma to take better self-control of their lung condition.
Many people may not realise that asthma is a condition of inflammation and by using a regular low dose of inhaled anti-inflammatory medicine (also known as ‘the preventer inhaler’) this can help keep symptoms at bay. Asthma is sometimes not taken seriously because of its episodic nature; however, many healthy living pharmacies have experts that are equipped to coach people on how to not only use their inhaler but also the right one at the right time.
There are 7 steps to using an inhaler and it’s not easy to remember all of these steps ‘we’re all human after all and mistakes can happen’. This is why every time a person sees a non-judgemental health care professional like a pharmacist, they should ideally demonstrate their technique.
Poor inhaler technique can mean a person gets little medicine to the lungs which can result in a person potentially going onto have more regular breathless, cough or chest tightness moments; this can impact on overall quality of life.
Many people that illustrate technique on the TV, on the web, or in paper press get it wrong and this why community pharmacy teams are behind the #RightInhalerImage campaign. People with lung conditions deserve to know what good inhaler technique looks like and this should be normalised in media around us.
Children and adults should also know that in asthma the blue ‘emergency’ inhaler should be replaced by images of ‘the preventer’ (usually brown, red, pink, purple, yellow) inhaler as this is the inhaler that’s usually used on a daily basis. Metered dose inhalers, sometimes called ‘the puffer’ inhaler should also include a spacer device as research has shown this can help improve more of the medicine reaching the lungs.
Healthy Living pharmacies are usually open long hours (including weekends); some GP practices will also have pharmacists who can support the asthma nurse or GP too as part of a multi-disciplinary team.
Always remember to ‘Ask your Pharmacist’.
Pharmacy page Pharmacy – Healthy London Partnership
Inhalers Inhalers – Healthy London Partnership
Latest updates
Right Inhaler Image Campaign Poster IPCRG 2022
2021 campaign evaluation:
Right Inhaler Image Campaign Poster PCRS 2021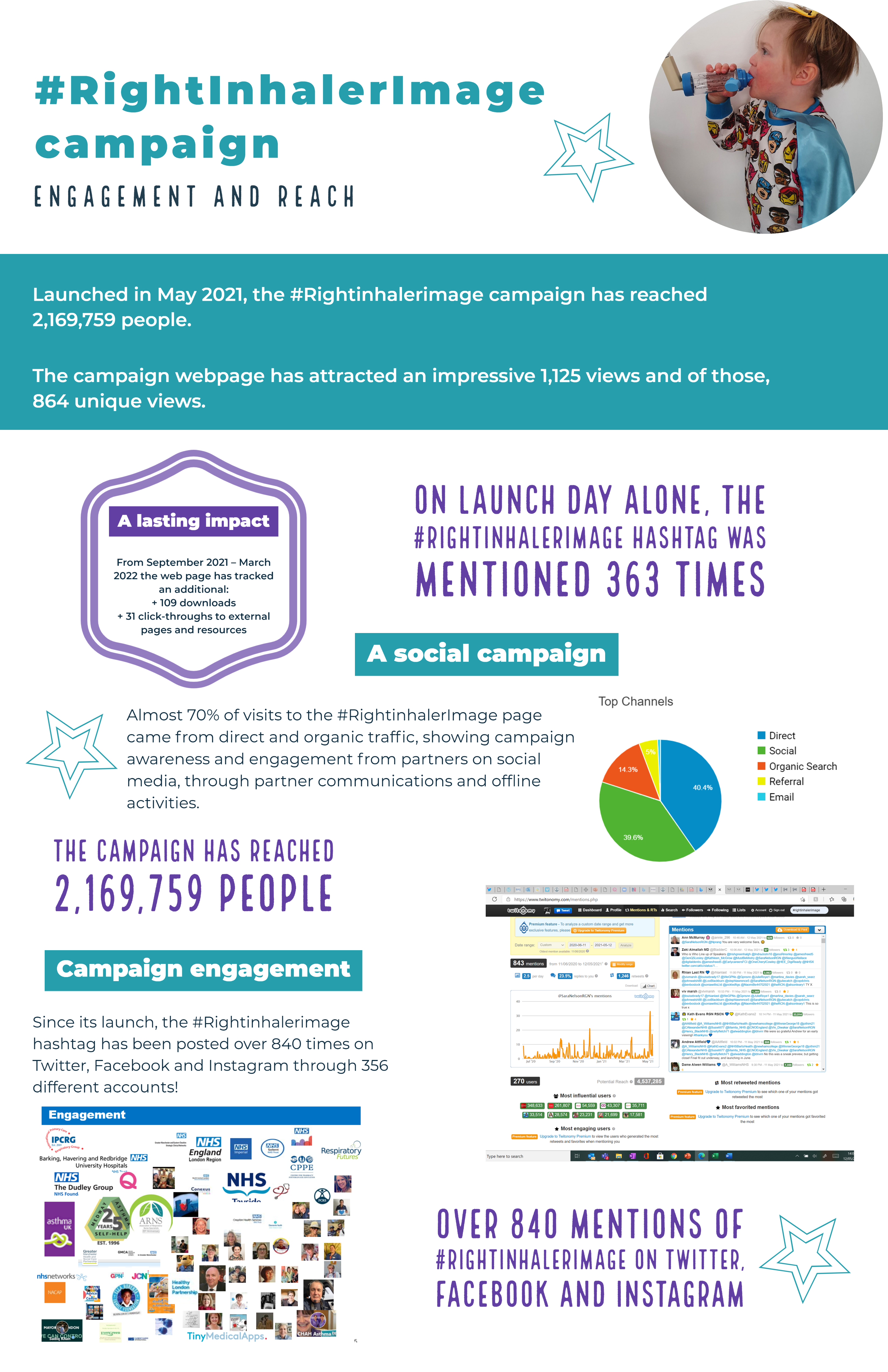
#RightInhalerImage campaign update
Read about the exciting next phase of the campaign, led by the International Primary Care Respiratory Group (IPCRG) here.
Team wins National Primary Care respiratory Award
In September 2021, the CYP Asthma team were delighted to be awarded the Most Patient Centred Poster Award for our ‘Kickstarting the #RightInhalerImage Campaign’ poster, during the Primary Care Respiratory Society (PCRS) 2021 Respiratory Conference. View the poster here.